In the quiet hours of the night, while the world sleeps, our brains engage in a profound cleansing ritual that scientists are only beginning to understand. Recent groundbreaking research has illuminated the critical role of cerebrospinal fluid in purging toxic waste from the brain during sleep, particularly the notorious beta-amyloid proteins implicated in Alzheimer's disease. This discovery not only transforms our understanding of sleep's purpose but opens exciting new pathways for combating neurodegenerative disorders.
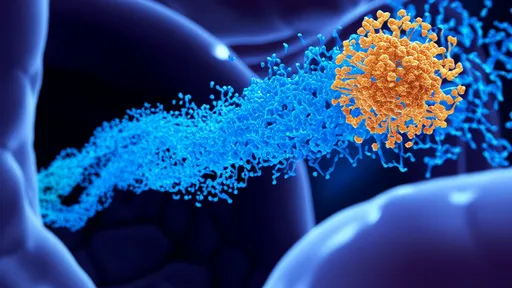
The cerebrospinal fluid, often viewed as merely a protective cushion for the brain, has emerged as a dynamic cleaning system. During deep sleep, the brain experiences synchronized slow waves of neural activity. These waves create a pulsating effect, much like a gentle tide washing over sandy shores, that drives the cerebrospinal fluid to rhythmically flow through brain tissue. This nightly ablution appears to be nature's way of maintaining cognitive health by clearing accumulated metabolic debris.
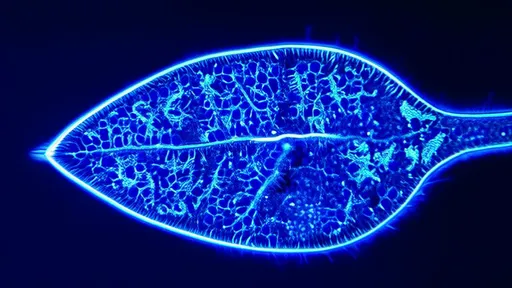
Researchers using advanced neuroimaging techniques have observed this process in action. Through simultaneous EEG and MRI scans, they've captured the beautiful choreography between neural activity and fluid movement. As neurons fire in coordinated slow waves, they create space between cells, allowing cerebrospinal fluid to flush through brain tissue and carry away toxic proteins. This discovery fundamentally changes how we perceive sleep's function - not merely as a period of rest, but as an active maintenance cycle essential for brain health.
The implications for Alzheimer's research are particularly profound. Beta-amyloid proteins, which accumulate as plaques in Alzheimer's patients, appear to be cleared primarily during this nightly cleansing process. When sleep is disrupted or shortened, this cleaning mechanism becomes less effective, potentially allowing toxic proteins to build up over time. This may explain why chronic sleep problems are strongly correlated with increased Alzheimer's risk later in life.
What makes this discovery especially remarkable is its potential for therapeutic applications. While much Alzheimer's research has focused on directly targeting amyloid plaques, this new understanding suggests that enhancing the brain's natural cleaning system might be equally important. Researchers are now exploring whether improving sleep quality or developing methods to stimulate cerebrospinal fluid flow could help prevent or slow neurodegenerative disease progression.
The relationship between sleep stages and cleaning efficiency presents another fascinating dimension. Deep non-REM sleep, characterized by slow brain waves, appears to be particularly effective for initiating the cerebrospinal fluid pulses. This explains why the first half of the night, when deep sleep predominates, may be most crucial for the brain's cleaning cycle. As we age, when deep sleep naturally decreases, this may contribute to increased vulnerability to cognitive decline.
Beyond Alzheimer's disease, this cerebrospinal fluid cleaning system likely plays a role in other neurological conditions. The accumulation of various toxic proteins is implicated in Parkinson's disease, Lewy body dementia, and other neurodegenerative disorders. Understanding how to optimize the brain's self-cleaning mechanism could have broad implications for brain health across multiple conditions and throughout the lifespan.
Practical applications of this research are already emerging. Sleep hygiene takes on new importance when understood as essential not just for daily functioning but for long-term brain maintenance. The research also suggests potential for non-invasive interventions, such as auditory stimulation during sleep to enhance slow waves and thereby improve cerebrospinal fluid flow. Early studies show promising results in both improving sleep quality and potentially enhancing protein clearance.
However, many questions remain unanswered. Researchers are still working to understand the precise mechanisms that coordinate neural activity with fluid flow. The relationship between different sleep stages, the role of various neurotransmitters, and how this system changes with age and disease all require further investigation. What's clear is that we're witnessing a paradigm shift in how we understand the relationship between sleep, brain function, and neurodegenerative disease.
The discovery of the brain's nightly cleaning system represents one of the most significant advances in neuroscience in recent years. It connects seemingly separate fields - sleep medicine, neurology, and gerontology - through a unifying mechanism that explains why sleep is so vital for brain health. As research continues to unfold, we may find that optimizing this natural cleaning process holds the key to preventing some of the most devastating neurological conditions affecting millions worldwide.
For now, the research offers both scientific insight and practical wisdom. The ancient intuition that sleep healing has found modern scientific validation. Those hours of slumber are not wasted time but an essential maintenance period during which our brains perform critical housekeeping. This understanding gives new meaning to the importance of prioritizing quality sleep - it's not just about feeling rested tomorrow, but about preserving cognitive function for years to come.
By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025